Restoring durable AV graft flow upon diagnosis of recoil post-PTA
GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface is not authorized for the treatment of stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts in Canada.
A case study using the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface*,†
Challenge
A 70-year-old male with a history of diabetes mellitus, renal cell cancer and end stage kidney disease presented with prolonged bleeding and elevated venous pressures from his right brachial artery to axillary vein arteriovenous (AV) graft. The patient’s 6 mm polytetrafluoroethylene (PTFE) AV graft had been created eight months prior to presentation and had no history of previous interventions. On physical examination, the graft was pulsatile. A Doppler ultrasound evaluation revealed a brachial artery flow volume of 650 mL/min, with presence of an apparent venous anastomosis stenosis.
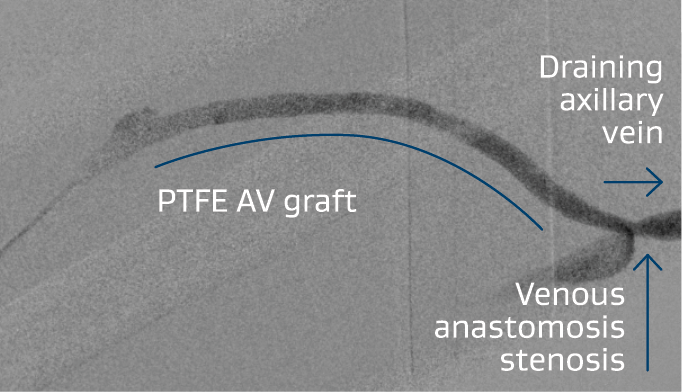
Figure 1: Right brachialaxillary AV graft with stenosis at the venous anastomosis.
Images courtesy of Daniel V. Patel, M.D. Used with permission.
Procedure
Given the clinical presentation, an angiogram was performed to confirm the presence of a stenosis at the venous anastomosis (Figure 1). The lesion was initially treated with percutaneous transluminal angioplasty (PTA) using an 8 x 40 mm BD® VACCESS® PTA Dilatation Catheter. Examination post-angioplasty revealed recoil at the venous anastomosis and that the graft was still pulsatile, so the decision was made to place a stent graft. An 8 x 50 mm VIABAHN® Device was advanced to the venous anastomosis (Figure 2) and deployed. This was then post-dilated with the 8 mm angioplasty balloon. A repeat contrast injection revealed successful deployment of the stent graft, with an improved thrill on physical examination (Figure 3).
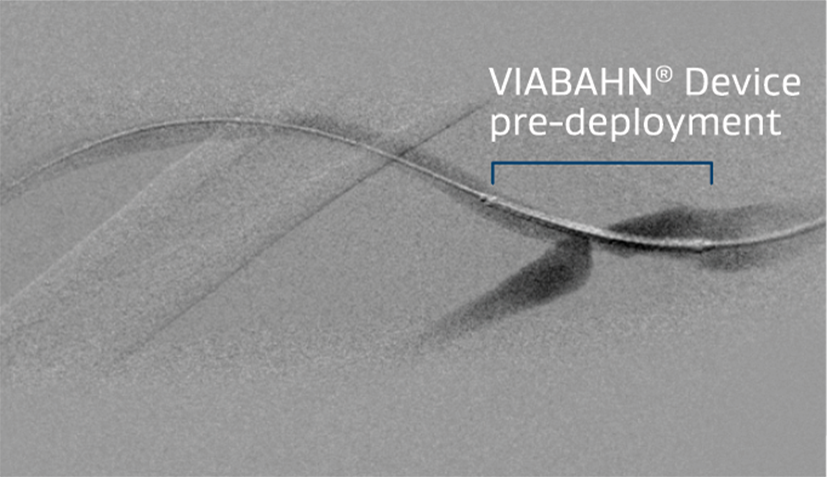
Figure 2: 8 x 50 mm VIABAHN® Device advanced across the venous anastomosis.
Images courtesy of Daniel V. Patel, M.D. Used with permission.
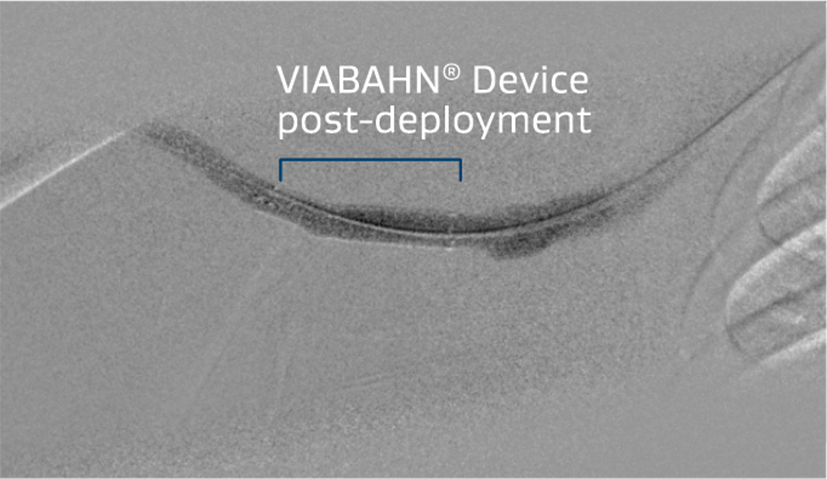
Figure 3: Improved flow and resolution of recoil post- VIABAHN® Device placement.
Images courtesy of Daniel V. Patel, M.D. Used with permission.
Result
Physical examination confirmed a significant improvement in the thrill through the graft, with a reduction in pulsatility. A repeat Doppler examination revealed improvement in the brachial artery flow volume to 980 mL/min. The patient successfully returned to hemodialysis later that afternoon for treatment. There was a reduction in his venous pressures and a resolution of his access bleeding issues.
The patient presented 13 months later due to difficulty with graft cannulation. An angiogram revealed no significant stenosis within the graft, and the cannulation areas were marked for the dialysis staff. Of note, the VIABAHN® Device placed at the venous anastomosis remained patent as confirmed by angiography (Figure 4).
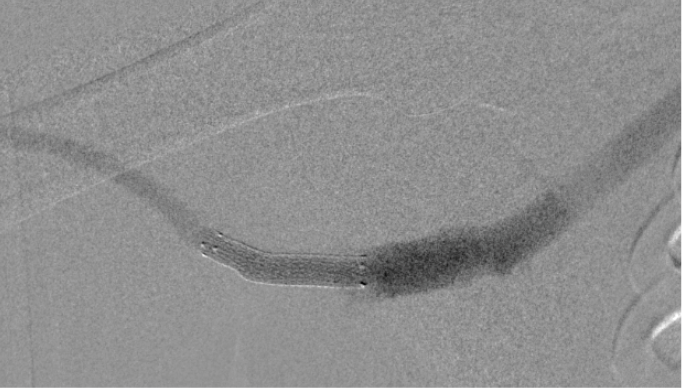
Figure 4: Patent VIABAHN® Device 13-month post-placement.
Images courtesy of Daniel V. Patel, M.D. Used with permission.
Case takeaways
Management of the venous anastomosis is essential in maintaining dialysis graft patency. Balloon angioplasty at the venous anastomosis may yield near-term recoil, restenosis and graft thrombosis. Stent grafts can offer a more durable treatment option. The Gore REVISE Clinical Study demonstrated that the VIABAHN® Device was superior to balloon angioplasty in maintaining access patency.1
In this case, the VIABAHN® Device remained patent for over 13 months without any episodes of thrombosis, allowing for a durable access management option at this site of recurrent stenosis. For dialysis patients with frequent access dysfunction, this could make a meaningful impact on their care and help to extend the longevity of their graft patency.
Related case studies
* As used by Gore, Heparin Bioactive Surface refers to Gore's proprietary CBAS® Heparin Surface.
† Also referred to as the GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface in some regions.
1. W. L. Gore & Associates, Inc. GORE® VIABAHN® Endoprosthesis versus Percutaneous Transluminal Angioplasty (PTA) to Revise Arteriovenous Grafts at the Venous Anastomosis in Hemodialysis Patients. (GORE REVISE Study, AVR 06-01). Flagstaff, AZ: W. L. Gore & Associates, Inc; 2012. [IDE Final Clinical Study Report]. G070069.
The outcomes and observations reported are based on individual case experience and the patients treated. The steps described here may not be complete, and are not intended to be a replacement for the Instructions for Use (IFU) or the education, training and professional judgment of health care providers (HCP). HCPs remain solely responsible for making decisions about patient care and the use of medical technologies.
Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available. RXOnly
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery de novo and restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 7.5 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery in-stent restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 6.5 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in iliac artery lesions up to 80 mm in length with reference vessel diameters ranging from 4.0 – 12 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is also indicated for the treatment of stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts.
CONTRAINDICATIONS: The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is contraindicated for non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system. Do not use the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II.
INDICATIONS FOR USE IN CANADA: The GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface is a flexible, self-expanding endoluminal prosthesis for endovascular grafting of peripheral arteries.
CONTRAINDICATIONS: The GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface is contraindicated for non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system. Do not use the GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II

