GORE® CARDIOFORM Septal Occluder Clinical Data

Gore REDUCE Clinical Study Long-Term Outcomes
After over a decade of clinical use, 90,000+ devices sold* globally and 2,069 patient years of data for patent foramen ovale (PFO) closure,1,2 the GORE® CARDIOFORM Septal Occluder continues to demonstrate its well established safety profile and clinical performance.
The REDUCE Study is the only U.S. Investigational Device Exemption (IDE) trial that achieved its primary endpoint, and over five years showed a significant reduction in recurrent stroke across PFO anatomies over medical therapy alone.†,‡,§
Gore REDUCE Clinical Study five-year results demonstrate PFO closure provides safe long-term prevention of recurrent stroke
- Published in the New England Journal of Medicine (NEJM), the REDUCE Study continues to show the largest reduction in recurrent ischemic stroke in all PFO shunt sizes over medical therapy alone. ‡,2
Long-term results highlight GORE® CARDIOFORM Septal Occluder’s demonstrated record of patient safety and effective defect closure.
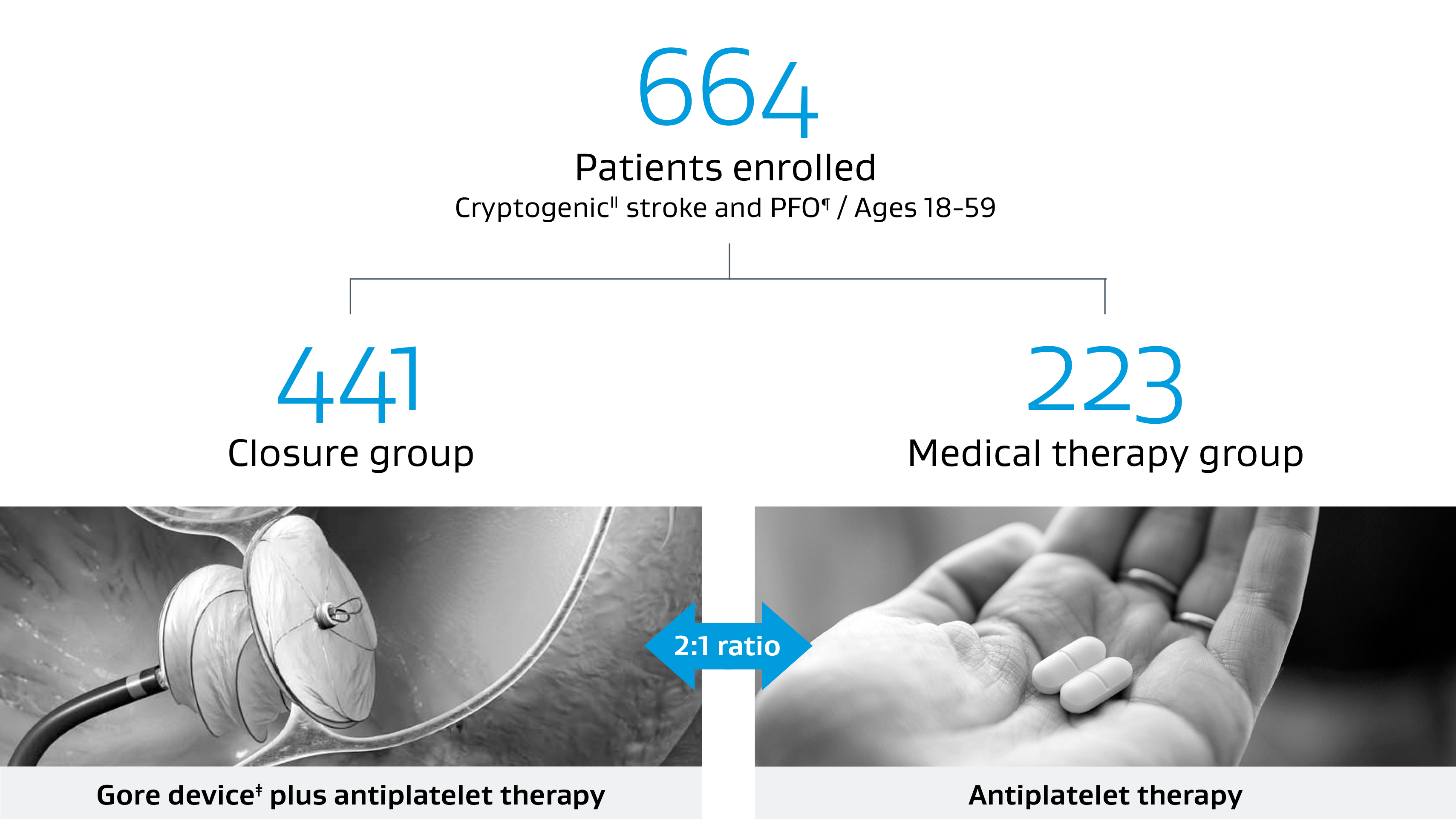
Robust trial design
The REDUCE Study evaluated whether PFO closure with a Gore device plus antiplatelet therapy reduces the risk of stroke compared to antiplatelet therapy alone.
- Prospective, randomized, multinational open-label trial.
- Standardized antiplatelet therapy for the medical arm. Trial designed to minimize medical therapy confounding.
- Prospective, 2-year MRI imaging.
- Inclusive of all PFO types. ‡,1
- 63 investigational sites in seven countries.
Key takeaways from long-term follow-up REDUCE study at five years:
- In carefully selected patients, PFO closure with the GORE® CARDIOFORM Septal Occluder device significantly reduced the risk of recurrent stroke compared to antiplatelet therapy alone over a five-year period.
- 69% relative reduction in recurrent stroke versus medical management alone at five-year median follow-up.‡,2
- Low risk of early device or procedure-related complications, none late.
- No reported cardiac erosions including through long-term follow-up.
- The majority of atrial fibrillation and atrial flutter cases were non-serious, early onset and resolved.2,3
- The benefit of closure persists long term with a low risk of late stroke, atrial fibrillation or other complications.
A leader in safety
Long-term results continue to demonstrate a legacy of patient safety with 2,069 patient years of data.1,2
Low risk of device or procedure-related serious adverse events (SAEs)2
No new device or procedure-related SAEs at five years.
The data presented are from separate and independent clinical studies with different patient populations and interventions and thus are not a direct head-to-head comparison.
REDUCE (median 5 years)2 | RESPECT (median 5.9 years)4 | |
|---|---|---|
| Device-related SAE | 6 (1.4%) | 13 (2.6%) |
| Procedure-related SAE | 11 (2.5%) | 12 (2.4%) |
Low risk of atrial fibrilation (AFib)1,2
The REDUCE trial showed only 0.5 percent device or procedure-related serious AFib.
The data presented in the table is from separate and independent clinical studies with different patient populations and interventions and thus are not a direct head-to-head comparison.
REDUCE (median 5 years)2 | RESPECT (median 5.9 years)4 | |
|---|---|---|
| Serious device or procedure-related AFib | 2 (0.5%) | 2 (0.4%) |
| Subjects with post-implant AFib or flutter who had a recurrent stroke | 1 (0.2%) | 1 (0.2%) |
No reports of erosion
REDUCE (median 5 years)2 | |
|---|---|
| Cardiac erosion | 0 |
Trusted closure performance
99% Effective closure
across PFO anatomies at 24 months**,††
Unmatched secondary stroke prevention
The REDUCE Study continues to show the largest reduction in recurrent ischemic stroke in all PFO shunt sizes over medical management alone.‡,2
Stroke reduction data
Ischemic stroke reduction relative to medical management.
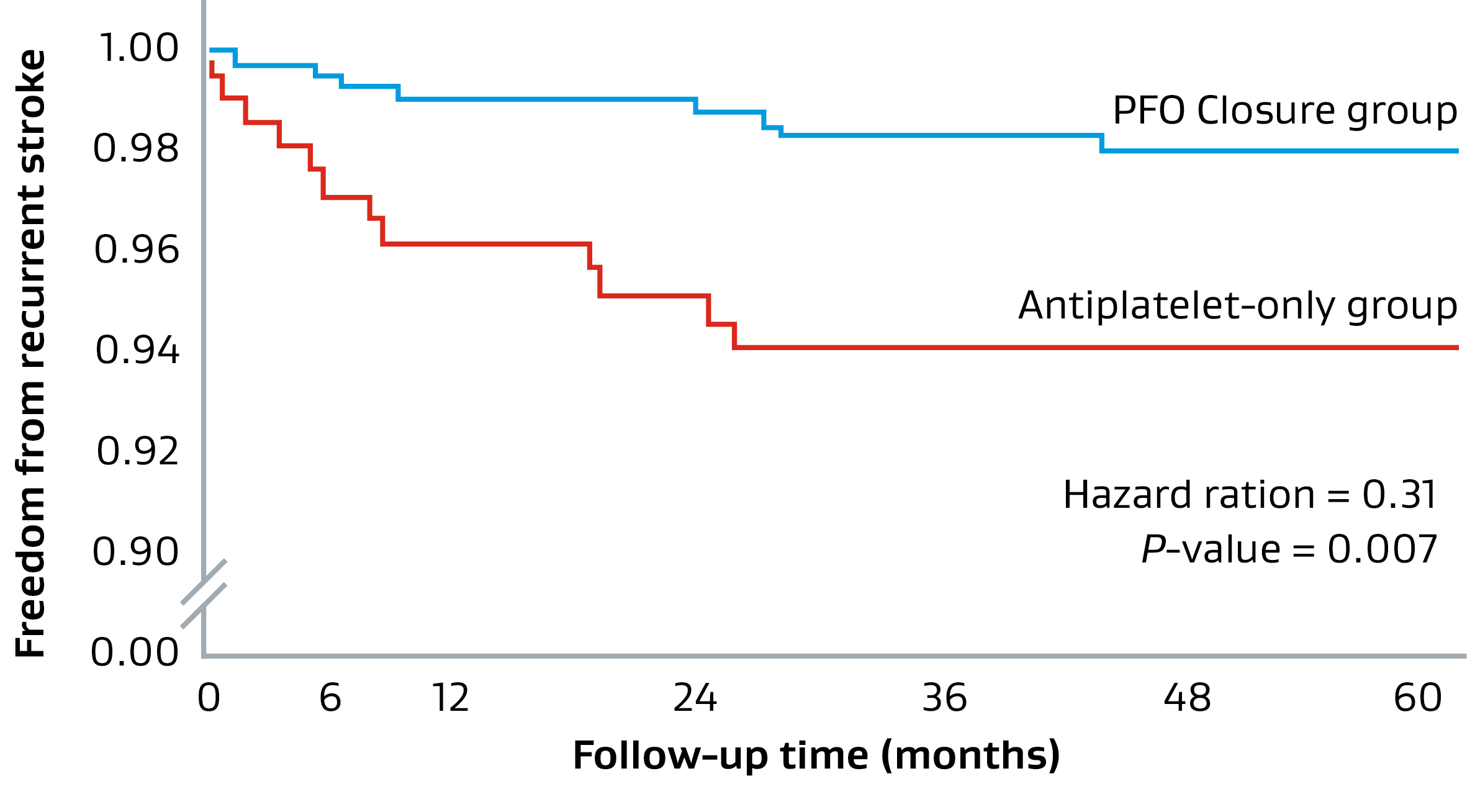
69% Stroke reduction
with PFO closure†,2 plus medical therapy versus medical therapy alone
Compelling real-world results
Number of patients needed to treat to prevent one recurrent ischemic stroke at five years.
25
REDUCE Study
Extended follow-up (median 5.0 years)2
* Data on file 2024; W.L. Gore & Associates, Inc; Flagstaff, AZ.
† In patients with a PFO and history of cryptogenic stroke.
‡ The REDUCE Study determined safety and efficacy of PFO closure with the GORE® CARDIOFORM Septal Occluder or GORE® HELEX® Septal Occluder plus antiplatelet medical management compared to antiplatelet medical management alone in patients with a PFO and history of cryptogenic stroke. All PFO anatomies were eligible for inclusion into this study within indicated sizing parameters of the Instructions for Use.
§ REDUCE is the only U.S. IDE trial that achieved its primary endpoint, and over five years showed a significant reduction in recurrent ischemic stroke across PFO anatomies over medical therapy alone.
II Cryptogenic diagnosed as: No stenosis > 50 percent or ulcerated plaque in relevant intra- or extra-cranial vessels, no atrial fibrillation or high-risk source of cardioembolism, non-lacunar (based on neuroimaging), no evidence of hypercoagulable disorder, no other known cause of stroke.
¶ PFO confirmed by transesophageal echocardiography (TEE / TOE) with bubble study demonstrating right-to-left shunt at rest or during Valsalva maneuver. Patients with PFO eligible regardless of shunt size or presence of atrial septal aneurysm.
** Effective closure defined as freedom from large shunt > 25 bubbles as detected by transthoracic echocardiography adjudicated by Echo Core Lab.
†† Data on file 2020; W. L. Gore & Associates, Inc.; Flagstaff, AZ
- Søndergaard L, Kasner SE, Rhodes JF, et al.; Gore REDUCE Study Investigators. PFO closure or antiplatelet therapy for cryptogenic stroke. New England Journal of Medicine 2017;377(11):1033-1042.
- Kasner SE, Rhodes JF, Andersen G; Gore REDUCE Clinical Study Investigators. Five-year outcomes of PFO closure or antiplatelet therapy for cryptogenic stroke. New England Journal of Medicine 2021;384(10):970-971.
- Kasner, SE. Long-term outcomes with patent foramen ovale closure or antiplatelet therapy for cryptogenic stroke. Presented virtually on November 7, 2020, at European Stroke Organisation & World Stroke Organisation conference.
- Sayer JL, Carroll JD, Thaler DE, et al.; RESPECT Investigators. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. New England Journal of Medicine 2017;377(11):1022-1032.
In some jurisdictions, ASPIRIN is a trademark of Bayer Intellectual Property GmbH or its affiliated companies.
ABBOTT and AMPLATZER are trademarks of Abbott Laboratories.
Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available. RXOnly
INDICATIONS FOR USE IN THE U.S.: The GORE® CARDIOFORM Septal Occluder is a permanently implanted device indicated for the percutaneous, transcatheter closure of the following defects of the atrial septum: ostium secundum atrial septal defects (ASDs); patent foramen ovale (PFO) to reduce the risk of recurrent ischemic stroke in patients, predominantly between the ages of 18 and 60 years, who have had a cryptogenic stroke due to a presumed paradoxical embolism, as determined by a neurologist and cardiologist following an evaluation to exclude known causes of ischemic stroke.
INDICATIONS FOR USE IN CANADA: The GORE® CARDIOFORM Septal Occluder is a permanently implanted device indicated for the percutaneous, transcatheter closure of atrial septal defects (ASDs), such as ostium secundum and patent foramen ovale.
CONTRAINDICATIONS: The GORE® CARDIOFORM Septal Occluder is contraindicated for use in patients: unable to take antiplatelet or anticoagulant medications such as aspirin, heparin or warfarin; with anatomy where the GORE® CARDIOFORM Septal Occluder size or position would interfere with other intracardiac or intravascular structures, such as cardiac valves or pulmonary veins; with active endocarditis, or other infections producing bacteremia, or patients with known sepsis within one month of planned implantation, or any other infection that cannot be treated successfully prior to device placement; with known intracardiac thrombi.