Cephalic arch stenosis
Challenge
- A 70-year-old male on hemodialysis (HD) via a left brachiocephalic fistula created three years previous
- One de-clotting procedure three months previous, where a cephalic arch stenosis was identified and treated successfully with balloon venoplasty
- Increased venous pressures on HD two months later – therefore repeat procedure / intervention
Image courtesy of Robert Jones, MD. Used with permission.
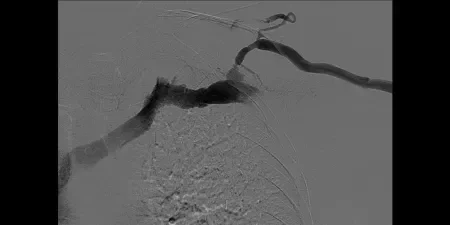
Procedure
Direct left brachiocephalic fistula access. Venography demonstrated recurrent cephalic arch stenosis. Venoplasty to 7 mm with a high-pressure balloon and recoil stenosis. Upsizing of sheath access. Deployment of a 7 mm x 5 cm GORE® VIABAHN® Endoprosthesis, and post-dilatation.
Image courtesy of Robert Jones, MD. Used with permission.

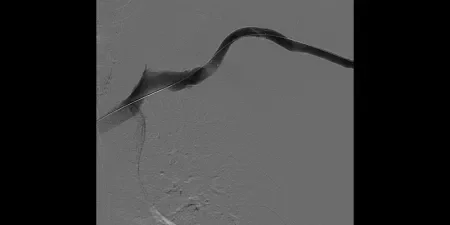
Result
A good result was achieved and the subclavian / axillary vein was not compromised. Follow up venography at three months demonstrated on-going patency.
Image courtesy of R Jones, Interventional Radiologist, Birmingham, UK. Used with permission.
Case Takeaways
- Symptomatic and recoil cephalic arch stenosis requires a durable solution to restore and maintain patency
- Cephalic arch stenosis is a notoriously difficult area to treat in the dialysis circuit. High rates of treatment failure and recurrent stenosis are seen with venoplasty alone.
- When venoplasty fails the GORE® VIABAHN® Endoprosthesis offers a durable solution as it conforms very well to the anatomical configuration of the arch without kinking
- It is possible to accurately deploy a GORE® VIABAHN® Endoprosthesis in the cephalic arch without significant compromise to the axillary vein
- Device introduction from the fistula access (as opposed to femoral access) provides more precise control during deployment and allows more accurate positioning as the GORE® VIABAHN® Endoprosthesis deploys distal – proximal
- ESVS guidelines recommend that endovascular treatment with stent grafts should be considered for the treatment of cephalic arch stenosis (Recommendation 63)1
1. Schmidli, J. et al., Vascular Access: 2018 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS), European Journal of Vascular and Endovascular Surgery 2018 Jun;55(6):757-818